HBF eyes alternative hospitals for east coast members after shock Healthscope move to slug out-of-pocket fee
Hospitals giant will charge members of Bupa and the HBF-affiliated Australian Health Service Alliance out-of-pocket fees of up to $100 after the insurers refused to join rivals in footing soaring medical costs.

HBF will be forced to find alternative hospitals for nearly 300,000 east coast members affected by Healthscope’s shock move to slug more than 6.5 million Australians with out-of-pocket fees after their insurers refused to join rivals in footing soaring medical costs.
Healthscope said patients covered by Bupa and the Australian Health Service Alliance would have to pay the unprecedented “hospital facility fee” of up to $100 a day to access its 38 hospitals from late next month because of the insurers’ “failure to sustainably cover the cost of patient care”.
“Unfortunately, Bupa and the AHSA refuse to fund Healthscope hospitals at a level that allows us to remain viable,” it said.
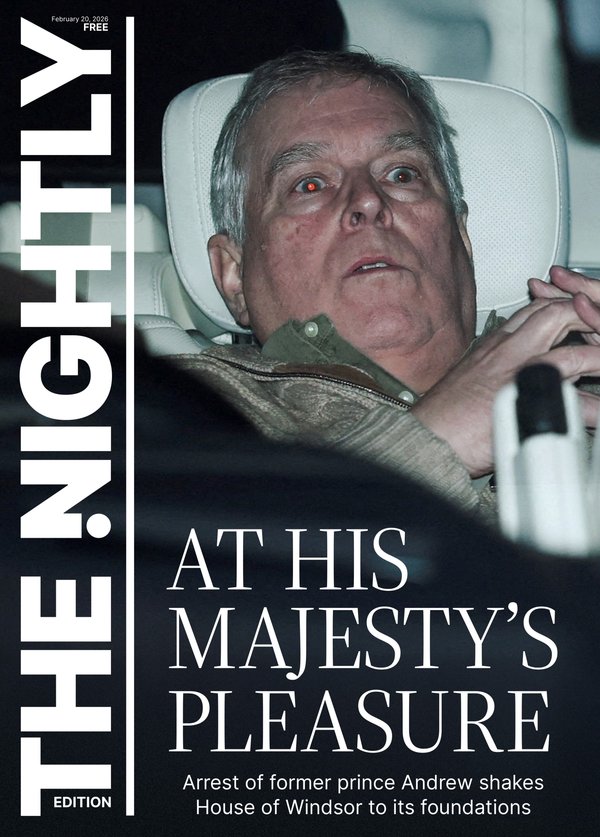
Sign up to The Nightly's newsletters.
Get the first look at the digital newspaper, curated daily stories and breaking headlines delivered to your inbox.
By continuing you agree to our Terms and Privacy Policy.The group, owned by private equity giant Brookfield, also suggested that members who wanted to avoid the fee switch to other insurers who have fallen into line with Healthscope and agreed to give it more money.
The AHSA covers HBF and more than 20 other the not-for-profit insurers representing 2.5 million members, though the impact on WA’s dominant insurer is limited to its growing interstate membership of nearly 300,000.
HBF chief executive Lachlan Henderson said his group was disappointed by the Healthscope move, saying it would cause “anxiety and uncertainty for people trying to plan their healthcare”.
“Our membership base in WA is unaffected by this move given a separate contract arrangement with Healthscope, however we will be working to inform our members in other states about their options to access other contracted hospitals to avoid these fees,” Dr Henderson said.
The private health insurance industry has reacted with fury, with peak body Private Healthcare Australia lashing Healthscope for “a deeply unethical move”.
“Brookfield was only ever in the Australian hospitals market for the short term,” chief executive Rachel David said.
“It is trying to squeeze out as much profit as possible before it abandons Healthscope hospitals, potentially making private healthcare unaffordable in the process.
“Targeting patients is a new low. I have never seen a hospital group do this before. This will cause great distress and uncertainty for thousands of people trying to plan healthcare across Australia right now.”
Bupa said it was “shocked and disappointed” by the Healthscope move, accusing it of “a public scare campaign designed to unsettle patients”.
The group said it had made “reasonable offers” of additional funding to Healthscope, including one last week, but they had all been rejected.
“Unfortunately, the increase Healthscope has been seeking is not sustainable nor appropriate, the impacts of which has the potential to flow-on to higher health insurance premiums for our customers,” Bupa said.
The AHSA called a move “a disgrace”, accusing Healthscope of breaking a new binding services agreement that took effect in only March.
“At AHSA our focus is to ensure members have access to quality care, but it also needs to be affordable in the long term,” chief executive Andrew Sando said.
“There is no point having a private health system if no one can afford it.
“We understand the pressures that private hospitals are under and have worked to balance their needs while being conscious of the potential impact on premiums that private health insurance members pay, remembering the funds we represent are not-for-profit and member-owned.”
From November 26, members of Bupa and the alliance will be slugged $100 for an overnight hospital stay and $50 for same-day admissions.
Patients receiving chemotherapy, renal dialysis or palliative care will be exempt, as will those in day mental health and rehabilitation programs.
Bupa claims to service 4 million members, while the more than 20 insurers covered by the alliance have 2.5 million members.
Healthscope and other operators have warned they will have to close hospitals without additional funding from health insurers to meet their rising costs of treating patients.
Insurers have countered they would have to lift insurance premiums to cover the extra contributions, potentially putting coverage out of reach of Australians already labouring under rising cost-of-living pressures.
Nonetheless, Medibank Private, NIB and HCF were reported last month to have agreed to out-of-cycle funding payments in the “tens of millions of dollars” for Healthscope.
Healthscope said on Tuesday these funds had “improved their funding of patient care in Healthscope hospitals”, adding they had “worked constructively ... to reach these agreements which are in the best interests of patients”.
Healthscope’s chief executive Greg Horan insisted the group had been trying to avoid charging the out-of-pocket fee, but “Bupa and the Alliance funds have left us with no choice”.

“We are introducing this fee due to these insurers’ failure to sustainably cover the cost of patient care in our hospitals,” he said.
“Members of Bupa and the Alliance insurers ... should also be aware that they have the option of switching their cover to any of the other health insurers who fund our hospitals sustainably.
“If they do this they will not be subject to the new fee, and so long as they move to a comparable product, they should not need to re-serve waiting periods.”
Mr Horan denied Healthscope was profiteering, insisting the new fee did not cover its full funding gap and claiming there had been “a $1 billion profit swing” from hospitals to insurers in the recent years as the former battled rising costs, particularly for labour.
He said Healthscope was conscious of not hitting up patients more than it had to given household pressures but accused the insurers of letting down members,
“As an insurer, your primary focus is to fund your members’ healthcare, and when you fail to do so, you’re falling short of your primary purpose”.