Best diet for children: Do ultra-processed foods cause bad behaviour and can a diet change banish tantrums?
Does a bad diet cause tantrums in kids? One family put this theory to the test. What happened next should give every parent pause for thought.

For the past three years, peace has been in short supply for Kate and Mike Rawlings as the behaviour of their older child has spiralled out of control.
Isobel, now eight, would routinely turn meal times at their Northampton home into a battlefield, repeatedly getting up and down from the table and shouting at Kate, 42, a dietitian, and Mike, 43, a sales manager.
Simple requests to come to the table could result in unprompted bursts of rage that often descended into screaming meltdowns, where Isobel would storm out of the room, slamming doors and on occasion lashing out at her sister, Sophie, four.
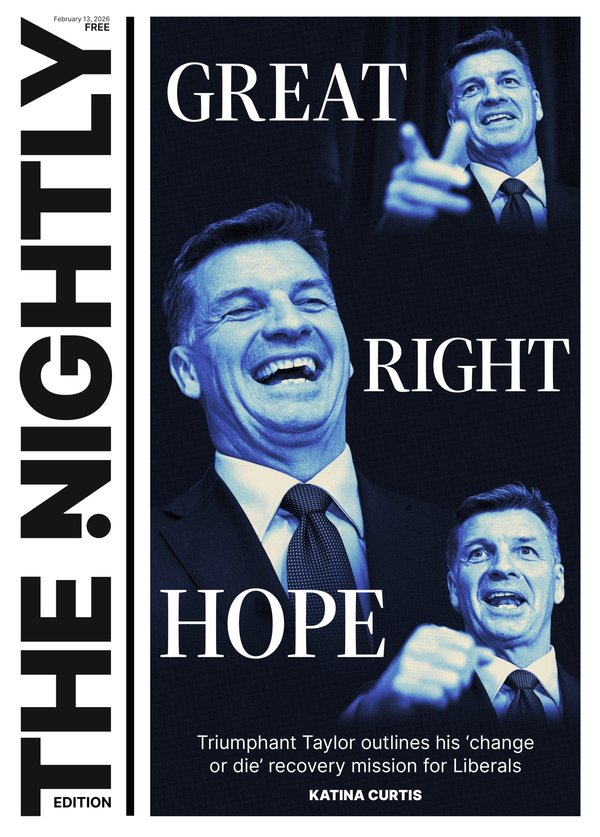
Sign up to The Nightly's newsletters.
Get the first look at the digital newspaper, curated daily stories and breaking headlines delivered to your inbox.
By continuing you agree to our Terms and Privacy Policy.“Isobel’s behaviour had become progressively worse over the past two or three years and life was becoming exhausting and very frustrating,” Kate said.
“At first we thought she might have been copying naughty children at her school, and then we wondered if she was acting out of jealousy for her sister.”
But then, in April, Ms Rawlings read something on social media that stopped her in her tracks.
A British TV fitness coach, Joe Wicks, had speculated that the sugary junk food he’d eaten as a child could have been directly linked to his former unruly and often naughty behaviour.
His comments were seen as controversial by some and went viral on social media.
Mr Wicks had to issue a clarification that poor diet alone can’t cause disorders such as ADHD (attention deficit hyperactivity disorder, which can run in families and can lead to seemingly ‘naughty’ behaviour) but he said: “I do believe food has a massive impact, whether you have ADHD or not.”
“I think it really impacts our mood and our ability to sit and focus, and even our energy and our mental health.”
Reading this made Ms Rawlings wonder if diet could be affecting Isobel’s behaviour, too.
“Her uncontrolled bursts of anger had been happening more and more frequently, and we were all on tenterhooks trying to avoid triggering an explosion and not knowing what to do when she kicked off,” she said.
“Isobel seemed to hold things together at school but her temper would explode when she got home. It wasn’t just meal times — she would take any opportunity to pick a fight with Sophie, and then go completely crazy if she couldn’t get her own way, screaming and slamming doors.”
Bedtimes too were a big problem and just getting Isobel up and ready for school each morning presented another area of conflict.
“The only way to tempt her to eat breakfast was with a croissant in front of the TV,” Ms Rawlings said.
As a qualified dietitian working with troubled adults in a mental health unit, she admits to being embarrassed that a possible food connection hadn’t previously occurred to her.
“When family life is so stressful, you’ll do anything to keep the peace, and although I was trying to find time to cook family meals from scratch, highly processed products — sauces, ready meals and snacks — had been creeping into the weekly shopping basket.”

So could Isobel’s explosive temper tantrums really be rooted in her diet?
“More and more research is uncovering links between poor behaviour and diet in children — and that’s not just down to sugar — but due to lots of other elements in the diet from additives to the type of cooking oil used,” says Dr Alex Richardson, a nutritional neuroscientist and visiting research fellow at Bournemouth University, who is a specialist at investigating the links between food and behaviour.
To test how much of an impact diet can have, Ms Rawlings decided on a mini-trial.
Dr Richardson sent a strengths and difficulties questionnaire to fill in about Isobel’s behaviour.
It is used in scientific studies to assess emotional and behavioural difficulties in children.
She then analysed the results.
This assessment put Isobel in the top 10 per cent of children for emotional problems, and in the top 5 per cent for hyperactivity and difficulties with “conduct”.
Her antisocial behaviour score was at the top of the range.
Dr Richardson, who is also director of the independent charity Food and Behaviour Research, analysed the family diet and suggested changes based on scientific evidence that would hopefully improve Isobel’s behaviour.
For three weeks, the entire family adhered to Dr Richardson’s suggested meal plans and kept a daily diary for Isobel to see what impact it had.
The results came as a shock to everyone involved.
SUGAR SABOTEUR
“Of all the dietary changes you can make to try to improve a child’s behaviour, reducing sugar will usually have the most rapid — if not the most significant — impact,” Dr Richardson said.
“And my first observation on seeing Isobel’s food diary was the number of sugary foods she eats.”
Dr Richardson estimated Isobel was eating more than 40g of sugar per day, which is nearly double the recommended limit of 24g for children aged seven to ten.
She says: “Anyone — adult or child — who starts their day with highly processed sweet stuff, such as cereal or croissants, sets themselves up for a roller coaster of blood sugar peaks and troughs which make impulse control and concentration difficult. Studies show added sugar impairs the efficiency of mitochondria [tiny structures inside our cells] which power every cell of our body and brain.”

Studies, including one published in the Journal of Affective Disorders in 2019, have shown that high-sugar, high-fat diets can increase the risk of ADHD in children (characterised by hyperactivity, impulsiveness and inattention), while diets rich in vegetables and fruit appear to protect against these types of behaviour.
Research by Yale University published in the Journal of Pediatrics in 1995 found that sugary drinks triggered a rise in levels of the hormone adrenaline in children, which has separately been shown to lead to aggressiveness, restlessness and concentration difficulties.
THE SOLUTION: Dr Richardson advised Kate to remove or hide all sugary snacks, and include protein in each meal to ensure Isobel felt full and had less urge to snack between meals.
“Treats” such as low-sugar, oat-based biscuits could be offered no more than once a day, and highly processed white bread, cakes, crisps, sweet yoghurts and biscuits were off the table.
LACK OF NUTRIENTS
Ultra-processed foods, which are industrially produced, often contain lengthy lists of artificial ingredients.
Dr Richardson estimates that Isobel’s diet was closer to 80 per cent ultra-processed foods.
“Even a homemade sandwich counts as a UPF if it’s made with shop-bought white sliced bread and processed ham,” she said.
Dr Richardson warns that a diet high in UPFs will contain a lot of artificial additives and this could leave a child deficient in essential nutrients such as iron and zinc, which are known to be important for mood and behaviour — and deficiencies have been linked with ADHD-like behaviours and other behavioural problems.
“An early study found one type of artificial colouring reduced levels of zinc in children with ADHD, but not in children in the control group,” she said.
“Other evidence suggests some children may be particularly sensitive to artificial additives.”
Two studies by researchers at the University of Surrey (one in 1990, the other in 1997) found that some artificial colours (specifically a yellow food dye called tartrazine) increase ADHD symptoms and reduce zinc levels in children with ADHD, leaving children without ADHD unaffected.

Meanwhile, artificial sweeteners may upset the balance of the gut microbiome (bacteria and other microbes known to play a part in sending signals from the gut to the brain that help to regulate mood).
Similarly, some emulsifiers added to processed food to improve texture or extend shelf life are now thought to disturb the delicate balance of gut bacteria.
What’s more, a diet high in UPFs tends to be low in fibre (as processing strips away fibre) — and whereas children of Isobel’s age should eat about 15g of fibre per day, Dr Richardson said she was eating less than 5g a day.
Low-fibre food (whether savoury or sweet) is more swiftly digested and converted into sugar in the blood, potentially leading to mood swings — plus fibre is important for maintaining the gut microbiome.
“We now know how important a healthy gut microbiome is for mental and physical wellbeing, and how it cannot thrive on a low-fibre, ultra-processed diet,” Dr Richardson said.
THE SOLUTION: Kate was advised to remove all UPFs from Isobel’s diet, to switch to cooking meals from scratch, and to increase her intake of fruit, vegetables, nuts and whole grains to increase her fibre intake.
TOO MUCH ‘TOXIC’ OIL
Processed foods are usually made using seed oils (such as sunflower oil or soybean oil), which research now suggests can prompt inflammatory changes in the body and may influence behaviour.
Dr Richardson said: “Every time children eat crisps, biscuits or cakes they are filling themselves with what are essentially toxic fats,” explaining that highly processed fats are thought to make brain cell walls less flexible, impacting communication between them and in turn affecting mood.
THE SOLUTION: Kate was urged to reduce Isobel’s intake of fried foods, switch from using vegetable oils to olive oil or butter and add more oily fish (salmon, sardines, mackerel) rich in omega-3 fatty acids to her diet.
Dr Richardson says a daily supplement may be advisable if a child is unwilling to eat oily fish.
She also notes that it could take up to three months for changes in dietary fats to impact Isobel’s behaviour, “because the brain is the last organ to recover when it has been deficient for some time”.
TOO MUCH DAIRY?
Isobel loves milk, bread and pasta, but “there’s a possibility that she could be sensitive to the specific proteins in cow’s milk and gluten which could be affecting her behaviour”, Dr Richardson said.
“This is a controversial link — which has only been reported anecdotally and through animal studies — but sometimes it is worth experimenting with goat’s milk and gluten-free bread and pasta to see if it helps.
“There is lots of research trying to pin down the mechanisms at play, but when we digest gluten or a protein in cow’s milk called casein we produce protein fragments called peptides which activate the same receptors in the body and brain as opioid drugs,” she said.
“While most people don’t seem to have problems with this, the theory is that these “opioid peptides” make gluten and milk products seem highly addictive to some sensitive individuals — enough to trigger disruptive behaviour or mood swings, and so strong cravings for these foods.”
THE SOLUTION: Dr Richardson predicted that if Isobel was sensitive to these peptides, then swapping cow’s milk for goat’s and temporarily removing gluten from her diet might prompt worse behaviour initially as her system reacted to withdrawal, but that her behaviour might then become more settled.
THE RESULTS
After three weeks of following Dr Richardson’s recommendations, Kate filled in the strengths and difficulties questionnaire again.
Dr Richardson analysed the results.
She said: “When I compared the results from the first behaviour questionnaire and the second, even I was stunned by the results. All the scores had dropped into the category of “average” for a child of her age.
“It is quite remarkable to achieve this change in behaviour in such a short space of time, as it can take up to three months for a dietary change to impact behaviour.
“But this adds support to the growing evidence that food and behaviour are inextricably linked — and some children are more sensitive to the effects than others.
“We all benefit from eating better, but the research shows that those who benefit the most are those having difficulties with mood, behaviour, sleep or the ability to learn.”
She said: “Simple dietary changes really can have a powerful impact, and they provide a safe and effective way to complement other approaches to difficult behaviours — in both children and adults.”
FAMILY’S VERDICT
Kate says: “At first, it seemed like a lot of effort for no gain. Isobel resolutely refused to eat the overnight oats and pancakes I made for breakfast without loads of sugar or chocolate spread — she kept asking for her usual breakfast croissant. The nuts I put in her lunch box came back intact but with the salt licked off.
“And for the first week, even though Isobel told me she was really keen to find out if new foods made her “less angry” — her behaviour remained volcanic. In fact, one particularly violent doorbanging outburst resulted in a glass panel being smashed.
“But in the second week, I started preparing mini breakfast omelettes with red pepper each evening for a grab-and-go breakfast and the girls reluctantly started to accept popcorn instead of crisps and low-sugar oat biscuits [2g of sugar per biscuit compared to 5g for a chocolate digestive] as an occasional treat.
“And despite never having eaten fish, Isobel slowly came around to the idea of fish fingers [in a gluten-free crumb].
“During the second week, there was at least one episode where Isobel shouted and refused to comply with simple requests or grabbed her sister to make her cry, but there were signs of nicer behaviour, too.
“At the end of that second week, Isobel was awarded “star of the week” for working hard at school — that’s never happened before!
“And after a visit to my parents’ house, my mother spontaneously commented on how “lovely” Isobel had been. I was amazed.
“In the third week, I noticed Isobel was more settled at the dining table and wasn’t badgering me so much for sugary snacks. I had got so used to her waking up in a foul mood that I was caught by surprise when she willingly brushed her teeth one morning, and she even tidied away her toys at the first time of asking.
“This had to be linked to what she’s been eating.
“It’s been a tough three weeks, but I’m convinced these dietary changes did lead to improvements in her behaviour.
“It’s been time-consuming, and stressful, and my food shop is marginally more expensive, but it’s been worthwhile. Isobel is delighted the “experiment” has ended and keeps asking when we can go back to Mcdonald’s — but I’m hopeful we can keep up with some of the changes.”
Names have been changed

THE KEY CHANGES IN DIET
ISOBEL’S ‘OLD’ DIET
Breakfast: Weetabix or Rice Krispies with milk and sugar, or chocolate croissant.
Lunch: Ham or cheese sandwich with white or 50/50 bread, slices of red/yellow pepper, cucumber or apple; cocktail sausages; tube of flavoured yoghurt; packet cake slice or KitKat.
Dinner: Spaghetti hoops on toast with cheese; or sausages with waffle, sweetcorn and peas; or pasta with jar of sauce; or ready meal.
Snacks: Pom-Bear crisps, biscuits, chocolate mousse, crackers, breadsticks, rice cakes.
Drinks: Milk and water.
HER NEW DIET
Breakfast: Eggs with smoked salmon; or goat’s milk yoghurt; or overnight oats with fruit/nuts; or banana pancakes made with almond flour and egg.
Lunch: Goat’s cheese, chicken slices or peanut butter sandwich made with wholemeal gluten-free bread and fruit and vegetable sticks.
Dinner: Salmon or fish pie (made with goat’s milk); or shepherd’s pie; or gluten-free spaghetti bolognese; or roast chicken.
Snacks: Fruit smoothie; or oat cakes with nut butter; nuts/seeds; occasional homemade cakes.
Drinks: Goat’s milk and water.