THE NEW YORK TIMES: Is delaying menopause the key to longevity?
Scientists are studying how to keep the ovaries working longer — and potentially, prevent age-related diseases in the process.

In March, First Lady Jill Biden announced a new White House women’s health initiative that highlighted a seemingly obscure research question: What if you could delay menopause and all the health risks associated with it?
The question comes from a field of research that has started to draw attention over the last few years, as scientists who study longevity and women’s health have come to realize that the female reproductive system is far more than just a baby-maker. The ovaries, in particular, appear to be connected to virtually every aspect of a woman’s health.
They also abruptly stop performing their primary role in midlife. Once that happens, a woman enters menopause, which accelerates her aging and the decline of other organ systems, like the heart and the brain. While women, on average, live longer than men, they spend more time living with diseases or disabilities.
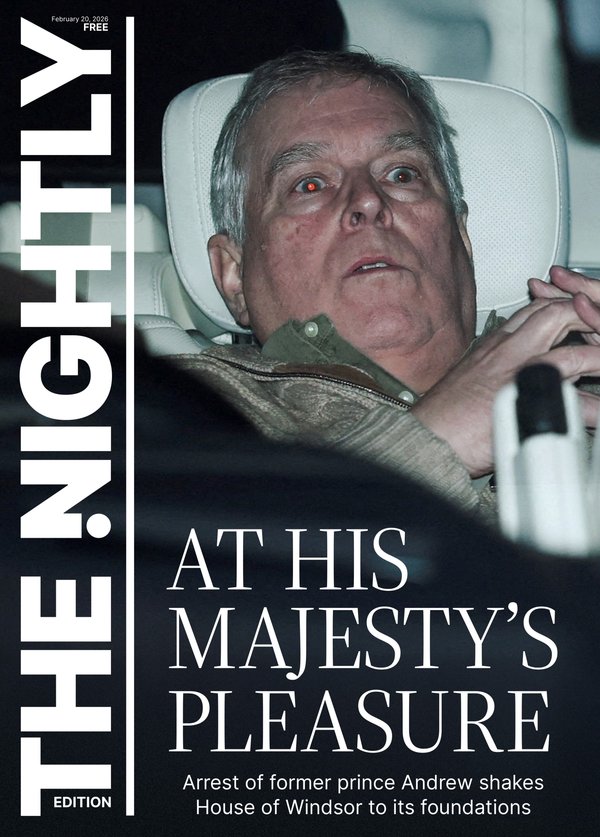
Sign up to The Nightly's newsletters.
Get the first look at the digital newspaper, curated daily stories and breaking headlines delivered to your inbox.
By continuing you agree to our Terms and Privacy Policy.The ovaries are “the only organ in humans that we just accept will fail one day,” said Renee Wegrzyn, director of the Advanced Research Projects Agency for Health, a government agency tasked with steering Jill Biden’s mission. “It’s actually kind of wild that we all just accept that.”
It is the ovaries’ truncated life span that also makes them such a promising site for experimentation. Researchers think that prolonging their function, better aligning the length of their viability with that of other organs, could potentially alter the course of a woman’s health — and longevity research overall.
Wegrzyn said she hoped the White House initiative, in which researchers and startups are competing for a slice of the program’s $100 million budget, would highlight the connection between menopause and longevity, while also attracting more funding and talent to the field.
“If you don’t think about ovarian function during aging,” said Jennifer Garrison, an assistant professor at the Buck Institute for Research on Aging, “then you’re kind of missing the boat.”
How the Ovaries Are Involved in Aging
The ovaries function like the control centre of “a complex network of signalling in a woman’s body,” Garrison said. Through hormones like estrogen and progesterone, as well as other chemicals, the ovaries communicate with and influence virtually every other organ. Scientists don’t yet know exactly how the ovaries do this, but what they do know is that when the ovaries stop functioning normally, all kinds of problems arise. In young women, for example, that can manifest as polycystic ovary syndrome, which increases the risk for metabolic conditions, heart disease, mental health problems and more.
As a woman’s eggs are depleted, eventually bringing menopause, the ovaries’ chemical communications seem to go quiet. That corresponds to an increased risk for dementia, cardiovascular disease, osteoporosis and other age-related diseases. The earlier a woman enters this life phase, the higher her risk for developing those conditions, and the shorter her life is likely to be. And in women who enter menopause prematurely because their ovaries are surgically removed, the risks for chronic conditions are greater still. That suggests that even after the ovaries stop releasing eggs in menopause, they may still be somewhat protective to a woman’s overall health, said Dr. Stephanie Faubion, the medical director of the Menopause Society. It’s just unclear how.
(BEGIN OPTIONAL TRIM.)
As of now, these connections are correlational. Scientists don’t know if the ovaries themselves are the drivers of health in aging, or if there is something else that accelerates aging that then leads to ovarian dysfunction, Faubion said. Studies have found that several factors, such as smoking, body mass index and adverse stressors throughout life, contribute to the early onset of menopause. Black and Hispanic women tend to hit menopause earlier than white women. Genetics might also play a role.
“Is the ovary just a marker of overall health? Or is it that the ovary is timing out and causing poor health?” Faubion said. “I mean, it’s chicken-egg.”
How Delaying Menopause Could Extend Life Span
There is some evidence, mostly in animals, that suggests prolonging ovarian function can improve health and increase longevity. In mice, for example, transplanting an ovary from a younger animal into an older one lengthens the older mouse’s life.
Scientists are now experimenting with different ways to prolong ovarian function and delay the onset of menopause in humans.
One company, Oviva Therapeutics, is in the early stages of testing — mainly in mice and cats — whether a pharmaceutical version of anti-Müllerian hormone (AMH), which modulates how many follicles mature in each menstrual cycle, could be used to reduce how many eggs are lost. (Typically, a woman loses dozens of eggs per cycle even though, in most cases, she only ends up ovulating one of them.)
Think of AMH as “a porous cloth that you cover around the ovary,” said Daisy Robinton, co-founder and CEO of Oviva, which is competing for some of the funding from the White House initiative. The level of AMH dictates the size of the holes in the cloth; if there are huge gaping holes (in other words, there’s low AMH), a bunch of eggs can leave in each cycle. But if there are only small holes (meaning there’s high AMH), fewer eggs can get out.
The idea is that if a woman loses fewer eggs, she can hold on to her ovarian reserves and the ovaries’ functionality for longer, Robinton said.
A clinical trial underway at Columbia University is also trying to slow the rate at which women lose their eggs. The study is testing the use of an immunosuppressive drug called rapamycin — which is used to prevent organ transplant rejection and has become a darling of the longevity movement — in women ages 35-45 to see how it affects their ovarian reserve. Rapamycin influences the number of eggs that mature each month, and the drug has been shown in mice to extend ovarian function.
The study is still ongoing, and the researchers don’t know which participants received the medication or a placebo, but the lead scientist on the trial, Dr. S. Zev Williams, said two patterns had already emerged: Some women appear to have a normal decline of ovarian reserve, which can be measured via ultrasounds and AMH levels, but in others, “it seems to have been altered,” he said. “So, you know, that’s promising.” Williams, an associate professor of women’s health at Columbia, is also applying for health agency funding.
The experts were explicit that the goal of this type of research was not to prolong women’s periods indefinitely, nor to make pregnancy possible at age 70 — though the treatments could potentially extend fertility.
The accelerated decline of the ovaries during midlife also makes them “a good model for being able to study aging, and being able to do so within a limited period of time,” Williams said. Other anti-aging scientists are also experimenting with rapamycin, for instance, but it’s virtually impossible to determine if the drug is extending human life without conducting a study over several decades. With the ovaries, researchers can see if there’s an effect much faster.
What’s more, “if we can understand why ovaries age prematurely and what’s driving that, that will almost certainly tell us something important about aging in the rest of the body,” Garrison said. “And then that, of course, becomes important not just for females, but also for males.”
This article originally appeared in The New York Times.
© 2024 The New York Times Company
Originally published on The New York Times