Washington Post: It’s official — pain hits women harder. Chronic pain more common and it’s not just hormones
The Washington Post: While some studies show no gender difference in the experience of pain, most suggest women are actually more sensitive to pain than men.

IIt is a common misconception that because women are able to give birth and routinely deal with sometimes agonising period cramps, they are somehow better able to tolerate pain than men. (It is probably one of the reasons women’s pain is so often dismissed or undertreated in medical settings.)
Nothing could be further from the truth. While some studies show no gender difference in the experience of pain, most suggest women are actually more sensitive to pain than men.
“It’s 180 degrees wrong. This has been studied hundreds and hundreds of times, and it’s sort of this zombie thing that won’t really die,” said Jeffrey Mogil, a Professor of pain studies at McGill University. “In my mind, this question of ‘who’s more sensitive to pain’ has been answered as clearly as anything in biology.”
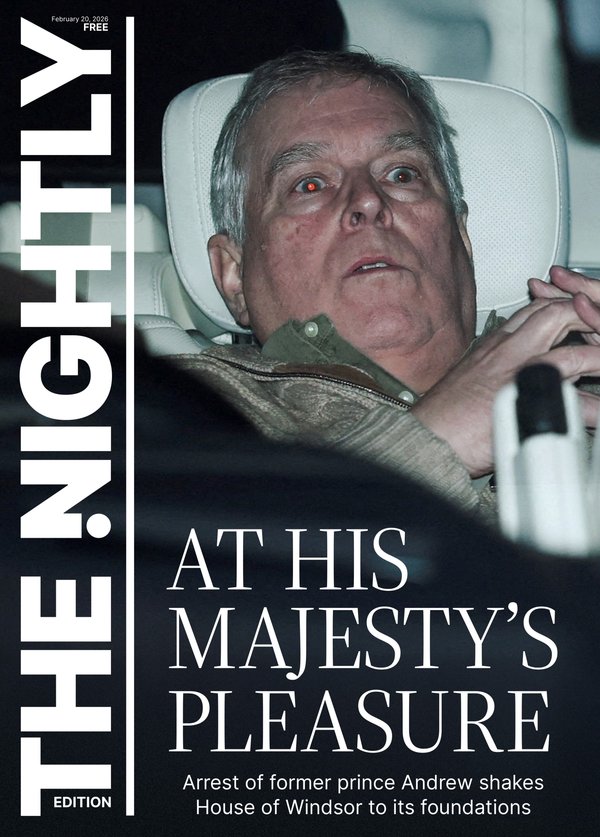
Sign up to The Nightly's newsletters.
Get the first look at the digital newspaper, curated daily stories and breaking headlines delivered to your inbox.
By continuing you agree to our Terms and Privacy Policy.The more important question that researchers are still trying to understand: Why do men and women experience pain differently? A quarter of American adults have chronic pain, which is pain that lasts longer than three months or beyond the expected healing time. And women are more likely to develop chronic pain than men.
Research suggests that everything from brain circuitry to immune cells involved in pain processing appear to be distinct between men and women — sometimes shockingly so, Mogil said. The good news is that as we learn more about how pain processing can vary, it might lead to better treatments.
“These studies are sending us a clear message that sex differences aren’t just stronger or weaker — they’re often entirely different wiring diagrams,” said Sean Mackey, the chief of the division of pain medicine at Stanford University. “And we need to be mindful of these differences between men and women when we’re treating them.”
Differences in pain biology

Earlier research has pointed to sex hormones as contributing to the experience of pain. During puberty, when dramatic changes of sex hormones occur, marked sex differences in the prevalence of clinical pain conditions begin to emerge. While roughly the same number of prepubertal girls and boys experience migraines, the prevalence more than doubles for women after puberty. Also, the severity of chronic pain symptoms can differ across the menstrual cycle.
But hormones do not tell the whole story. Even the way the brain is wired differs between men and women with the same chronic pain condition. The subgenual anterior cingulate cortex (sgACC) is a specific region of the brain that acts within the body’s natural pain relief system.
“Every kind of way we look at the brain system related to pain — either in terms of activity, connection to other areas of the brain, or oscillations — this area of the brain keeps coming up as being different in men and women,” said Karen Davis, a senior scientist at Krembil Brain Institute of the University Health Network who has studied the sgACC for over a decade.
Davis and her colleagues found that women with ankylosing spondylitis, a type of arthritis in the lower back, have greater connectivity between the sgACC and brain regions involved in processing sensory information compared with men. This unique brain circuitry could explain why women with the condition report more functional disability, higher disease burden and less response to treatment.
And sex differences in pain biology go beyond the brain, as Mogil’s lab has long known. As far back as 1996, Mogil and his colleagues started finding evidence of sex-specific genes that influence pain perception. Later on, they discovered startling sex differences in which immune cells contribute to pain. More recently, researchers have found that even nociceptors — the sensory neurons located in the skin, muscles, joints and internal organs that send pain signals to the brain — function differently in males vs. females, in humans and other animals.
“Even from the first step, the pain system appears to be sex dependent,” Mogil said. “Suffice it to say, people have found sex differences essentially at every level up the chain, from sensation to perception, so much so that it’s a little bit shocking.”
How these differences can affect treatment

About half of chronic pain conditions — including migraine, fibromyalgia, rheumatoid arthritis, osteoarthritis and irritable bowel syndrome — are more common in women. Only 20 per cent of chronic pain conditions are more common in men. (The rest are evenly split between the sexes.) One study of 42,249 adults across 17 countries found that the prevalence of chronic pain conditions was higher among women in both developed and developing countries.
Experts emphasise that more research characterising sex differences in pain is critical to improving pain management better tailored for both women and men. Currently, clinical trials that investigate treatments for chronic pain often fail to report sex effects or lack an adequate sample size for analysis. Historically, pre-clinical pain studies have overwhelmingly used male rodents.
One notable example is a protein called calcitonin gene-related peptide (CGRP), long assumed to play a role in migraines since it is elevated in the blood and saliva of patients during an attack. In 2009, scientists using male rats reported that CGRP does not elicit a migraine. A decade later, the study was repeated in both sexes, finding that, despite having no effect on males, CGRP creates a significant pain response in females.
Today, multiple drugs that block CGRP have been approved by the TGA for preventing and treating migraines. They have been game changers for many women, who are three times more likely to experience a migraine than men.
“There likely are important sex differences that we need to, not just find by circumstance, but we have to look for them,” Davis said. “Otherwise, the treatment aspect and translation to the clinic, we’re missing things and really doing a disservice to patients who are suffering from different types of pain.”
For instance, results from brain imaging studies can be used to tailor emerging treatments that target certain brain areas for stimulation, such as deep brain stimulation, which implants electrodes in specific regions of the brain to administer electrical currents. As with CGRP, certain molecules can be involved in modulating pain for one sex but not the other, which could lead to the development of targeted sex-specific drugs.
Tips for managing chronic pain
Not only do women experience more pain across the lifespan, but also they are more likely to have hard-to-diagnose pain conditions such as fibromyalgia and irritable bowel syndrome.
Here are some tips for women on advocating for better pain relief and management:
- If you don’t feel heard. Nearly one in four women report being treated “unfairly or with disrespect” by their health care practitioners, according to a recent survey. When visiting your doctor, come prepared with a journal of all your symptoms and a list of questions to ask.
- Speak honestly. Don’t downplay the severity of your symptoms. Be your own advocate by speaking truthfully about your pain, how it is affecting your daily life, and your treatment preferences.
- Ask a friend or family member to come along. Having a loved one there for support can help ease anxiety. Ask them to take notes and chime in with questions.
- Find the right fit. If a doctor makes you feel dismissed or uncomfortable — repeatedly, or even just once — don’t be afraid to look for a new provider.
“Don’t suffer in silence, and don’t give up,” Mackey said. “There is help out there.”