The New York Times (Science Times): Omicron, now two years old, is not done with us yet
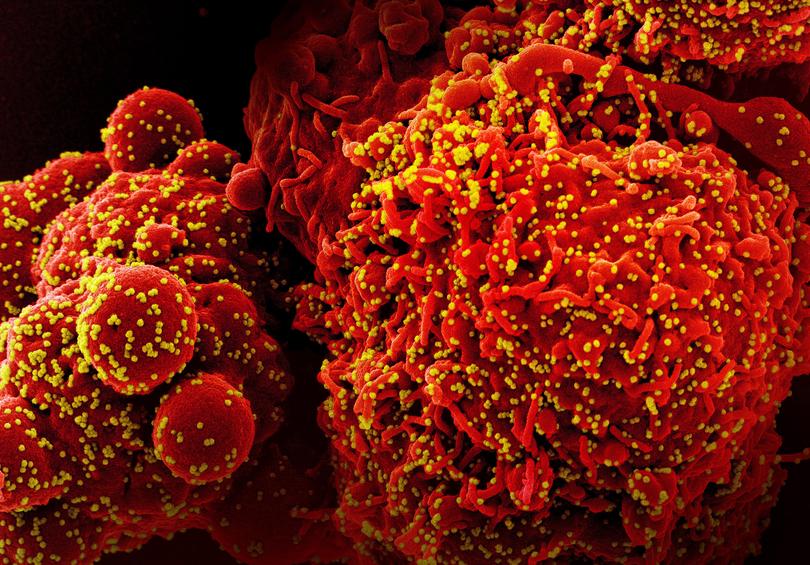
Omicron has proved to be not only staggeringly infectious, but also an evolutionary marvel. It has given rise to a number of descendants, which have become adept at evading immunity and finding new victims.

By November 2021, nearly two years after the coronavirus emerged in Wuhan, China, and spread across the world, the surprises seemed to be over. More than 4 billion people had been vaccinated against the virus, and 5 million had died. Two new variants, known as alpha and delta, had surged and then ebbed. As Thanksgiving approached, many Americans were planning to resume travelling for the holiday.
And then, the day after the turkey, the pandemic delivered a big new surprise. Researchers in Botswana and South Africa alerted the world that a highly mutated version of the virus had emerged and was spreading fast. Omicron, as the World Health Organization called the variant, swiftly overtook other forms of the virus. It remains dominant now, on its second anniversary.
In the two years since its emergence, omicron has proved to be not only staggeringly infectious, but also an evolutionary marvel, challenging many assumptions virologists had before the pandemic. It has given rise to an impressive number of descendants, which have become far more adept at evading immunity and finding new victims.
Sign up to The Nightly's newsletters.
Get the first look at the digital newspaper, curated daily stories and breaking headlines delivered to your inbox.
By continuing you agree to our Terms and Privacy Policy.“It was almost like there was another pandemic,” said Adam Lauring, a virus expert at the University of Michigan.

Lauring and other omicron watchers are trying to make sense of the past two years in order to prepare for the future. It’s possible that omicron will become a permanent part of life, steadily mutating like seasonal influenza.
When omicron first came to light, the United States and other countries wrongly believed they could stop its spread by barring travelers from South Africa. In reality, it had already spread far and wide. In a matter of days, Britain, Italy and Germany discovered omicron in positive COVID tests.
Omicron’s gift for spreading fast was the result of dozens of mutations. They altered the virus’ surface, so that antibodies produced by vaccines or previous infections could not stick tightly to it and prevent the virus from invading cells.
“It was the first virus to figure out in a major way how to escape immunity,” said Dr. Jacob Lemieux, an infectious disease specialist at Massachusetts General Hospital.
Lemieux and many other omicron experts suspect that the variant gained its new mutations while infecting a single person with a weak immune system. Immunocompromised people can only fight off some of the coronaviruses during an infection, allowing the ones that remain to acquire mutations that can thwart the immune system.
“It becomes like a laboratory for virus evolution,” said Peter Markov, a virus expert at the London School of Hygiene and Tropical Medicine.
As public health researchers tracked the omicron wave in late 2021, they saw a crucial difference from earlier surges. Compared with previous variants, omicron put a smaller fraction of infected people in the hospital. One reason was that so many people had immunity to earlier forms of the coronavirus. Our immune defences include not just antibodies, but special immune cells that can recognize and kill infected cells. This second line of defence held up even against omicron, preventing many of the new infections from becoming severe.
Still, omicron caused so many new infections — the initial wave infected almost half of all Americans, according to one recent estimate — that it still unleashed a devastating wave of hospitalizations.
The omicron surge hit the United States and most other countries in early 2022. China managed to hold back the waves with its “zero COVID” policy, but protests against its brutality grew so intense that President Xi Jinping dropped it abruptly in November 2022. The floodgates opened: Within a few weeks, more than 1 billion Chinese people contracted omicron, resulting in over 1 million deaths.
As omicron moved from person to person, its descendants gained more mutations. Sometimes two omicron viruses would wind up in the same cell, which would produce new hybrid viruses with a mix of their genes. One of these so-called recombinations hit the jackpot by mixing together two sets of evasive mutations. The result was a new hybrid called XBB.
The U.S. Centers for Disease Control and Prevention found that between October 2022 and September 2023, more than 80,000 people died of COVID, more than eight times as many as those who died of influenza.
XBB easily infected people and became dominant in the United States in early 2023.
Vaccine makers tried to keep up with omicron’s rapid evolution. In August 2022, the Food and Drug Administration authorized booster shots that targeted the BA.5 omicron variant, which was then dominant. In September 2023, the agency authorized an XBB shot. But XBB is now ebbing as a menagerie of even more evasive variants has evolved.
“Right now we’re in a period of chaos,” said Marc Johnson, a virus expert at the University of Missouri.
Several omicron experts said the chaos might soon end. In August, a variant called BA.2.86 emerged with a host of new mutations — most likely the result, once again, of evolution taking place in an immunocompromised person.
At first, BA.2.86 did not seem to live up to its genetic potential, failing to spread fast. “If genetics was all that mattered, it would have gotten its own Greek letter,” said Thomas Peacock, a virus expert at the Pirbright Institute in Woking, England. “But BA.2.86 was a bit of a damp squib.”
Over the past few months, however, the BA.2.86 lineage seems to have kicked into high gear, gaining a mutation that allows it to evade even more antibodies. JN.1, as this mutated form is known, has become the most resistant version of the coronavirus. It appears to be growing quickly in France, and may soon spread to other countries.

It is hard to predict the future path of a new variant like JN.1. Its success will depend on what kind of immune defences it encounters while spreading from host to host. At the outset of the pandemic, things were simpler because no one had developed immunity to the coronavirus.
“At the beginning, we were one big kindergarten,” said Michael Lässig, an evolutionary biologist at the University of Cologne.
Today, in contrast, most people on Earth have immunity of one form or another, whether from a natural infection, vaccination or both. “The virus sees a much more complex ecosystem,” Lässig said.
This worldwide immunity means that a smaller fraction of people will die than did at the start of the pandemic. Still, omicron’s toll remains heavy. The U.S. Centers for Disease Control and Prevention found that between October 2022 and September 2023, more than 80,000 people died of COVID, more than eight times as many as those who died of influenza.
As omicron continues to evolve, public health researchers still see a benefit to vaccinations. Justin Lessler, a researcher at the University of North Carolina, and his colleagues recently ran a projection of future COVID infections and concluded that annual vaccination campaigns could save up to 49,000 lives a year.
Those vaccines will be more effective if they’re updated to keep up with the evolving virus. But Katrina Lythgoe, a biologist at Oxford University, worries that their development will slow down as governments stop paying for genetic sequencing of new variants.
“If we don’t sequence things, then we won’t see them,” she said.
This article originally appeared in The New York Times.
© 2023 The New York Times Company
Originally published on The New York Times