The ‘tsunami’ of osteoarthritis: The alarming reason so many young people have worn-out joints
For years, the ‘wear and tear’ form of arthritis was primarily associated with the long-term effects of sport-related injuries, or simply getting older. Now, things have changed.

Before lockdown in 2020, Elizabeth Takyi had a thriving social life, a busy job and enjoyed regular gym sessions. “My life used to be great,” she says.
But today, the mother of three rarely leaves the house and needs a walking stick when she does.
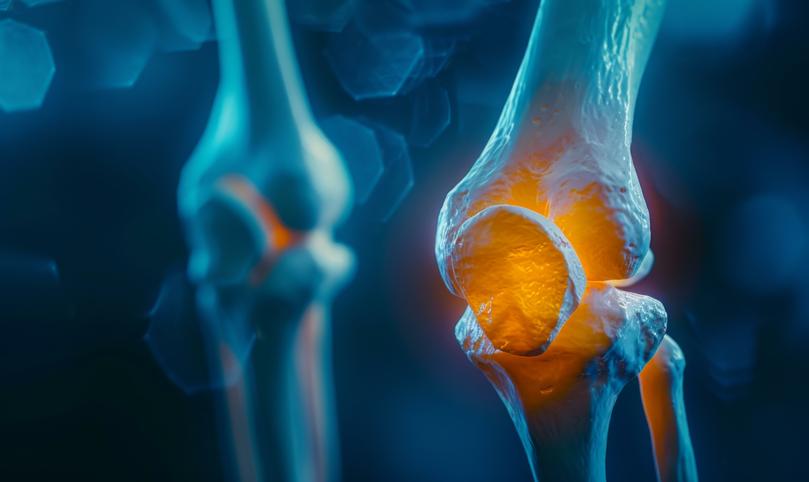
At 54, she is one of an estimated ten million people in the UK with osteoarthritis, a disease where cartilage – the tough fibrous material which acts as a “shock absorber” for our joints – gets worn down to the point where bones rub together, often causing extreme and crippling pain.
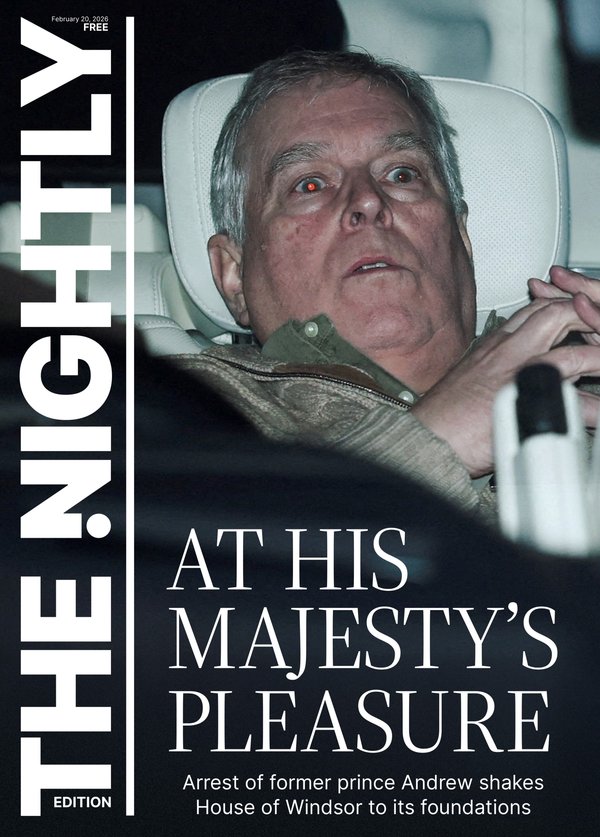
Sign up to The Nightly's newsletters.
Get the first look at the digital newspaper, curated daily stories and breaking headlines delivered to your inbox.
By continuing you agree to our Terms and Privacy Policy.For years, this “wear and tear” form of arthritis was primarily associated with the long-term effects of sport-related injuries, or simply getting older.
There can also be a family link – there are thought to be several hundred gene variations associated with the condition, and the more of these you have, the higher the risk.
Elizabeth Takyi is one of an estimated ten million people in the UK with osteoarthritis
Now experts are warning of a “tsunami” of osteoarthritis cases driven not just by Britain’s ageing population, but also by soaring rates of obesity that mean younger and younger people are being diagnosed with the disease.
“Obesity is a straight line to osteoarthritis – as we get heavier, our joints suffer more,” says Dr Wendy Holden, a consultant rheumatologist at North Hampshire Hospitals NHS Foundation Trust and medical adviser to the charity Arthritis Action.
“Knees are not designed to carry excess weight. It’s simple – like driving a heavy lorry over a bridge and making it collapse.”
And you don’t have to be morbidly obese to add to the strain on joints. In fact, any degree of being overweight “puts your body in an inflammatory state”, which increases the risk of osteoarthritis, says Dr Holden. “The more overweight you are, the higher the risk, and the longer that goes on, the worse the effects.
“But for every kilogram we carry above a healthy body weight, it has the impact of another 4-5kg going directly through our weight-bearing joints.’
That’s because the force exerted by additional weight gets amplified as it travels through joints – a kind of funnel effect. So for someone who is 20kg overweight, for example, the strain on their joints every time they take a step is roughly equivalent to 80-100kg, says Dr Holden.
A 2022 analysis of data from the National Joint Registry in England, Wales, Northern Ireland and the Isle of Man found that by 2060, demand for hip and knee replacements will increase by around 40 per cent due to the effects of soaring osteoarthritis rates.
The NHS already performs an estimated 100,000 knee replacement operations a year, plus 95,000 hip procedures. But the real burden could actually be much bigger, some experts fear.
“The figures we have for UK cases of osteoarthritis are probably the tip of the iceberg,’ says Dr Fiona Watt, a consultant rheumatologist and researcher at Imperial College London.
‘We’re probably undercounting because we’re relying on healthcare data that counts those given a specific diagnostic code for osteoarthritis. So if it is just recorded as joint pain, or if people don’t seek help and mistakenly think the condition is an inevitable part of ageing, then not all cases will be counted.”
In parts of the UK, she says, patients are waiting two years or more for joint replacement surgery as the NHS struggles to clear the backlog from the pandemic.
One of the most effective ways of offsetting the pain and discomfort caused by osteoarthritis is regular exercise. It both combats weight gain and boosts the strength of muscles capable of taking some of the strain off the damaged joints.
But many patients – like Elizabeth – who are already in pain and lacking mobility due to the condition struggle to get moving and do the exercise that could help.
It happens when cartilage – the tough fibrous material which acts as a “shock absorber” for our joints – gets worn down to the point where bones rub together, often causing pain
“If you have joint pain, you should be exercising more, not less, to strengthen the muscles around the joint and improve stability in the joint,”says Dr Holden. ‘You’re never too old to start exercising. Doing less leads to more weight gain and, in turn, more joint damage, so it becomes a vicious cycle.’

Moreover, being overweight is also thought to increase inflammation in the body, which can lead to osteoarthritis in non-weight bearing joints, such as the hands, too.
“We don’t currently have treatments that slow down the progression of osteoarthritis, so that’s a priority for researchers,” says Dr Watt, an adviser to the charity Versus Arthritis.
“Joint replacements are very effective in some people, but they are extremely costly and since Covid there are long waiting times for surgery. As cases increase, demand will keep going up.”
Elizabeth was told her weight was at least partly to blame for her condition. Before her diagnosis she’d suffered years of mild back pain, then her right hip and knee were affected.
As her pain worsened through 2019 and into 2020, she blamed sitting in one place for too long, while working from home during the Covid lockdown.
“When I bent down, it caused sharp hip pains so I couldn’t put socks on or tie shoelaces,’ recalls Elizabeth. She was also unable to walk to the park with her youngest daughter – having to drive the short distance instead.
One morning in June 2021 she woke barely able get out of bed, let alone walk, with “intense, spasm-like pain in my lower back’. A scan revealed severe osteoarthritis in Elizabeth’s hip.
“I was in shock as I always presumed it only affected elderly people,” she says.
At the time she was a size 14 and her BMI was in the overweight category. Plus, her mother also has the condition. “I was told to
lose weight to reduce the pressure on my joints and back,” says Elizabeth, a neurodiversity consultant from south-west London, who has two grown-up children aged 29 and 27, and a 14-year-old daughter.
“I lost a few pounds after the diagnosis, but now I’m a size 20 because while I’ve changed my diet, I struggled to exercise or move around much because of the chronic pain I was in.”
She was also diagnosed with osteoarthritis in her right knee in 2022 and in her spine earlier this year.
“It was a Catch-22 – the more exercise I did, the worse the pain got and sometimes my leg seized up,” says Elizabeth. “I tried to go to the gym and walk for 30 minutes every morning, but exercising left me in great pain the next day.” She adds that it is distressing to find herself so overweight as it has never previously been an issue.
Experts say although the outlook for the number of osteoarthritis cases is grim, there are emerging treatments that can help and – crucially – get patients moving again, so they can stop the vicious cycle of weight gain and more joint problems.
Healthy eating is essential – Dr Holden advises cutting out sugar and ultra-processed foods and switching to a Mediterranean-style diet (rich in fruit, vegetables, fish and olive oil).
Among the new treatments being investigated is hormone replacement therapy (HRT) – researchers at Oxford University are planning a trial with post-menopausal women with osteoarthritis, based on the theory that lower levels of oestrogen lead to weaker cartilage. Lower levels of oestrogen are also associated with increased inflammation in the body, which can make joint pain worse.
After a year’s wait, Elizabeth had her hip replacement a few weeks ago. “My social life is zero and my mental health has suffered due to everything I’ve been through,” she says. “I used to love making an effort to look and feel great, but I don’t feel like myself any more.
“But now I’ve had the operation I can try to rebuild my life. The pain from osteoarthritis has already improved – I can finally be hopeful again.”